Image Type
C2-C7 Translation
1) Description of Measurement
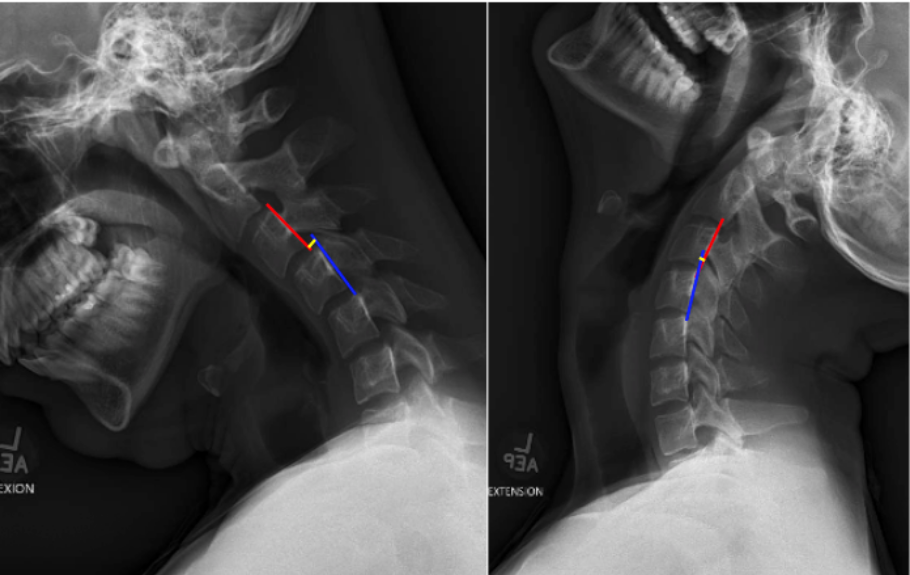
C2–C7 Translation quantifies the anterior–posterior (A–P) displacement of the cervical vertebrae between flexion and extension positions.
It is a dynamic measurement used to evaluate segmental instability across the subaxial cervical spine, particularly after trauma, degenerative changes, or postoperative conditions.
The method identifies abnormal intervertebral motion that may indicate ligamentous injury, facet subluxation, or instability of the functional spinal unit.
The measurement encompasses translation between vertebral bodies at each motion segment (C2–C7) during physiological flexion and extension.
2) Instructions to Measure
Obtain lateral cervical spine X-rays in both full flexion and full extension, ensuring visualization from C2 to C7.
Identify the vertebral levels to assess (typically C2–C3 through C6–C7).
For each motion segment:
Draw a vertical line along the posterior vertebral body margin of the superior vertebra (e.g., C4).
Draw a corresponding line along the posterior vertebral body margin of the adjacent inferior vertebra (e.g., C5).
Measure the horizontal (anterior–posterior) distance between these lines in flexion and extension views.Calculate translation as the difference between flexion and extension positions.
Record the translation value for each segment (in millimeters).The largest measured translation among segments (typically C4–C5 or C5–C6) is reported as the maximum translational motion.
Evaluate for instability:
Translation > 3.5 mm between flexion and extension is considered pathologic.
3) Normal vs. Pathologic Ranges
Normal Intervertebral Translation: ≤ 3.5 mm (<2 mm); physiologic motion, normal mobility
Abnormal/pathologic Intervertebral translation: > 3.5 mm; cervical instability
Key Point:
Translation > 3.5 mm or rotation > 11° between adjacent vertebrae indicates segmental instability—a hallmark of post-traumatic, degenerative, or iatrogenic pathology.
4) Important References
White AA, Panjabi MM. Clinical Biomechanics of the Spine. 2nd ed. Lippincott Williams & Wilkins; 1990.
Harris JH Jr, Edeiken-Monroe B. The Radiology of Emergency Medicine. 3rd ed. Williams & Wilkins; 1993.
Dvorak J, Panjabi MM. Functional anatomy, injury, and instability of the cervical spine. Spine. 1987;12(8):831–837.
Swartz EE, Floyd RT, Cendoma M. Cervical spine functional anatomy and the biomechanics of injury. J Athl Train. 2005;40(3):155–161.
Lee C, Woodring JH, Rogers LF, Kim KS. Sagittal alignment of the cervical spine: significance of posterior vertebral line discontinuity. AJR Am J Roentgenol. 1986;146(3):707–714.
5) Other info....
C2–C7 translation provides a dynamic functional assessment of cervical stability, supplementing static measurements like George’s Line and Spinolaminar Line.
Instability often arises from facet dislocation, degenerative spondylolisthesis, or ligamentous insufficiency (especially posterior longitudinal or interspinous ligaments).
A difference >3.5 mm in translation is one of White and Panjabi’s instability criteria and suggests loss of structural integrity.
Flexion–extension imaging should be performed only after acute fracture or dislocation has been excluded on CT.
Dynamic instability may present only in flexion-extension views, even when neutral alignment appears normal.
When measured across multiple levels, report the level of maximum translation (e.g., “C4–C5: 4.2 mm, unstable”).
Digital PACS tools improve precision; ensure magnification calibration using a radiographic scale marker.
In postoperative or fusion cases, residual translation helps evaluate fusion integrity or adjacent segment motion.