Image Type
Ullman’s Line
1) Description of Measurement
Ullmann’s Line is a radiographic parameter used to evaluate anterior vertebral translation (spondylolisthesis) at the lumbosacral junction (L5–S1).
It serves as a simple geometric reference for detecting anterior slippage of L5 relative to the sacrum by assessing the alignment between the L5 vertebral body and the sacral base.
The line provides a quick, qualitative and quantitative tool to detect low-grade spondylolisthesis and assess lumbosacral shear stability.
2) Instructions to Measure
Obtain a true standing lateral lumbar X-ray, ensuring visualization from L4 through the sacrum (S1).
Identify two key anatomical structures:
The superior endplate of S1 (sacral base).
The anterior inferior margin of L5.
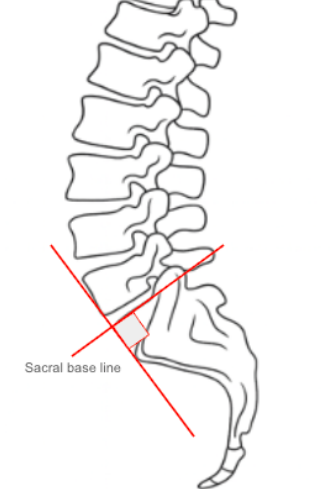
Draw the following reference lines:
Sacral Base Line: Extend a line along the superior surface of S1.
Perpendicular Line: Draw a line perpendicular to the sacral base line at its anterior corner.
Evaluate the position of the anterior-inferior corner of L5 relative to this perpendicular line:
Normal: The anterior-inferior corner of L5 is posterior to or just touches the perpendicular line.
Abnormal: If the L5 anterior-inferior corner crosses anteriorly beyond this line, it indicates anterior translation (spondylolisthesis).
For quantitative measurement, calculate the distance (in mm) that the L5 corner lies anterior to the perpendicular reference.
3) Normal vs. Pathologic Ranges
Normal alignment: L5 corner posterior to or tangent to the perpendicular line; indicates no anterior slip
Pathologic: L5 corner crosses anteriorly beyond perpendicular line; indicates anterior translation/spondylolisthesis
Progressive deformity: degree of anterior displacement increases with slip severity; correlates with Meyerding classification of spondylolisthesis
Key Point:
Any anterior crossing of Ullmann’s Line signifies abnormal vertebral translation—a hallmark of isthmic or degenerative spondylolisthesis.
4) Important References
Ullmann JB. The etiology and treatment of spondylolisthesis. J Bone Joint Surg. 1933;15(3):586–599.
Boxall D, Bradford DS, Winter RB, Moe JH. Management of severe spondylolisthesis in children and adolescents. J Bone Joint Surg Am. 1979;61(4):479–495.
Hresko MT, Labelle H, Roussouly P, Berthonnaud E. Classification of high-grade spondylolisthesis based on pelvic balance: the importance of sagittal alignment. Spine. 2007;32(20):2208–2213.
White AA, Panjabi MM. Clinical Biomechanics of the Spine. 2nd ed. Lippincott Williams & Wilkins; 1990.
Dubousset J, Shufflebarger H, Herring JA. Spondylolisthesis in children and adolescents. Spine. 1999;24(24):2640–2648.
5) Other info....
Ullmann’s Line is one of the earliest and most widely used radiographic methods for detecting spondylolisthesis and assessing lumbosacral stability.
It provides a static geometric check that complements quantitative slip grading (e.g., Meyerding Classification).
Especially useful in low-grade slips, where subtle anterior translation may not be visually obvious.
Best performed on standing radiographs to reflect weightbearing mechanics; supine films may underestimate translation.
Often used in combination with:
Meyerding’s Slip Percentage (quantitative slip grading).
Slip Angle / Lumbosacral Kyphosis (segmental angulation).
Pelvic Parameters (PI, PT, SS) for comprehensive sagittal balance assessment.
In severe slips, the L5 vertebral body may project significantly anterior to the perpendicular line, indicating advanced spondylolisthesis and potential need for surgical stabilization.
Clinical correlation: A positive Ullmann’s Line (L5 crossing anteriorly) typically coincides with pain, mechanical instability, or neurological symptoms in the lumbosacral region.