Image Type
Trunk Shift
1) Description of Measurement
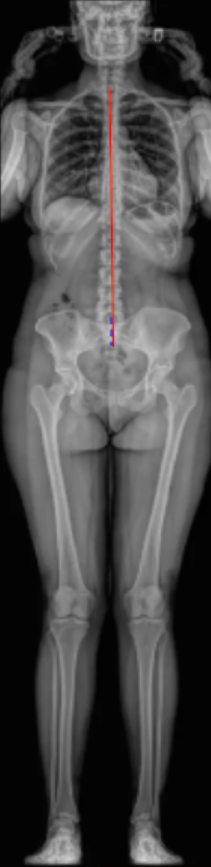
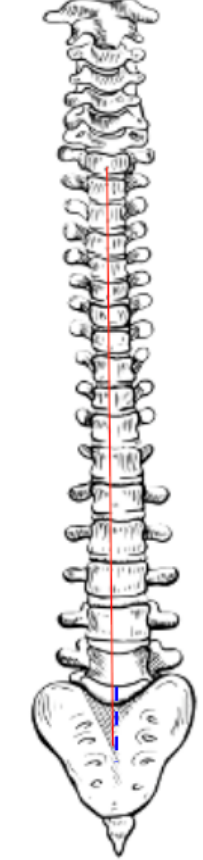
Trunk Shift quantifies the lateral displacement of the trunk relative to the pelvis in the coronal plane.
It is defined as the horizontal distance between the C7 plumb line (C7PL) and either the Central Sacral Vertical Line (CSVL) or the midpoint of the sacrum on a standing full-length spinal radiograph.
This parameter evaluates global coronal balance and complements the Cobb Angle and Coronal Balance in assessing scoliosis or spinal deformity.
An increased trunk shift indicates coronal decompensation, in which the head and thorax are not properly centered over the pelvis.
2) Instructions to Measure
Obtain a standing full-length AP or PA spinal X-ray with the patient in a neutral posture and both iliac crests visible.
Identify key landmarks:
C7 vertebral body center – mark the midpoint of the C7 vertebral body.
Center of the sacrum (S1 endplate) – mark the midpoint of the superior sacral endplate.
Draw the Central Sacral Vertical Line (CSVL):
A vertical plumb line extending upward from the midpoint of the sacrum (S1).
Draw the C7 plumb line (C7PL):
A vertical line dropped downward from the midpoint of the C7 vertebral body.
Measure the horizontal distance (in millimeters) between the C7PL and the CSVL or the center of the sacrum.
Note the direction of deviation (right or left).
A C7 plumb line that passes through or near the CSVL indicates balanced alignment.
Deviation to either side indicates coronal imbalance or trunk shift.
3) Normal vs. Pathologic Ranges
Normal Trunk Shift: ≤ 10 mm; balanced global alignment
Mild imbalance: 10-20 mm; slight trunk lean; often compensatory
Pathologic imbalance: > 20 mm; significant coronal decompensation; trunk shifted laterally
Severe imbalance: > 40 mm; marked coronal malalignment; often symptomatic or surgical indication
Key point:
A trunk shift > 20 mm is generally considered clinically significant coronal imbalance, often used as a radiographic criterion for decompensated scoliosis.
4) Important References
Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR. Coronal and sagittal balance in idiopathic scoliosis: does correction correlate with improvement in pain and function? Spine. 2005;30(7):682–688.
Schwab FJ, Lafage V, Boyce R, Skalli W, Farcy JP. Gravity line analysis in adult volunteers: age-related correlation with spinal parameters, pelvic parameters, and foot position. Spine. 2006;31(25):E959–E967.
O’Brien MF, Kuklo TR, Blanke KM, Lenke LG. Radiographic Measurement Manual. Memphis: Medtronic Sofamor Danek USA; 2008.
Hresko MT, Talwalkar VR, Schwend RM. Clinical practice guideline: evaluation and treatment of idiopathic scoliosis in children and adolescents. J Am Acad Orthop Surg. 2014;22(9):577–587.
Lafage V, Schwab F, Skalli W, Hawkinson N, Gagey PM, Ondra S. Standing balance and alignment in adult spinal deformity. Spine. 2008;33(14):1572–1578.
5) Other info....
Trunk shift reflects overall coronal compensation—whether the spine has re-centered over the pelvis despite curvature.
A positive shift (C7PL lateral to CSVL) indicates decompensation toward the curve’s convexity; negative indicates compensation toward concavity.
Postoperative trunk shift > 20 mm may correlate with shoulder asymmetry, rib prominence, or residual imbalance.
Often measured alongside Cobb angle and Apical Vertebral Translation (AVT) to assess both angular and translational deformity components.
Pre- and postoperative comparisons are useful for determining surgical effectiveness and postoperative balance restoration.
Low-dose EOS or stitched long-cassette standing films are preferred for precise measurement across the entire spine and pelvis.
Always report direction and magnitude (e.g., “Trunk shifted 25 mm to the right”).