Image Type
Rib-Pelvis Distance
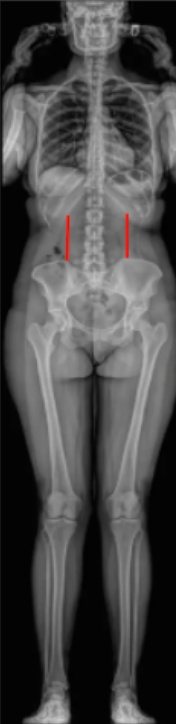
1) Description of Measurement
The Rib–Pelvis Distance (also called the Costopelvic Distance) is a linear coronal-plane measurement used in severe thoracic or thoracolumbar scoliosis to assess trunk height loss, spinal flexibility, and preoperative surgical planning.
It quantifies the vertical gap between the lowest rib margin and the iliac crest on the concave side of the deformity. A reduced distance indicates rib–pelvis impingement, which may contribute to flank pain, rib deformity, or restrictive pulmonary mechanics.
This measure provides an indirect estimate of curve stiffness and helps predict the amount of correction achievable with traction or surgical release.
2) Instructions to Measure
Obtain a standing full-length coronal (AP or PA) spinal X-ray, ensuring the thoracic cage, lumbar spine, and pelvis are fully visualized.
Identify the lowest rib margin on the concave side of the thoracolumbar curve (often the 12th rib, but confirm anatomically).
Identify the superior aspect of the iliac crest directly beneath that rib.
Draw a vertical line connecting these two points:
From the inferior border of the lowest rib → to the superior margin of the iliac crest.
Measure the shortest perpendicular distance between these two bony landmarks.
Document the side (right or left) and distance in centimeters or millimeters.
Repeat the measurement on both sides if asymmetry is present, as large differences reflect curve severity or truncal imbalance.
3) Normal vs. Pathologic Ranges
Normal Rib-Pelvis distance: > 3 cm; adequate trunk height; no costopelvic impingement
Mild narrowing: 2-3 cm; early loss of trunk height; mild scoliosis or postural change
Severe narrowing: < 2 cm; costopelvic impingement likely; significant thoracolumbar deformity
Rib-Pelvis contact: 0 cm/overlap; marked deformity or rigidity; often symptomatic and surgically significant
Key point: A distance < 2 cm often correlates with rigid curves, requiring more extensive surgical correction or osteotomy to restore trunk height and coronal balance.
4) Important References
Moe JH, Lonstein JE, Winter RB. Scoliosis and Other Spinal Deformities. Philadelphia: WB Saunders; 1978.
Bridwell KH, Lenke LG, Baldus C, Blanke K. Major curve correction and compensatory changes in idiopathic scoliosis. Spine. 1999;24(16):1679–1686.
Newton PO, Faro FD, Gollogly S, et al. Results of preoperative flexibility assessment in adolescent idiopathic scoliosis: are we doing enough? Spine. 2007;32(25):2658–2664.
Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR. Coronal and sagittal balance in idiopathic scoliosis: does correction correlate with improvement in pain and function? Spine. 2005;30(7):682–688.
Suk SI, Lee CK, Min HJ, et al. Determination of distal fusion level with segmental pedicle screw fixation in single thoracic idiopathic scoliosis. Spine. 1992;17(8):S89–S98.
5) Other info....
The Rib–Pelvis Distance is especially useful in thoracolumbar and lumbar scoliosis to gauge space for corrective maneuvers and to determine whether rib resection or spinal height restoration is necessary.
Reduction in this distance correlates with loss of trunk height, lumbar curve rigidity, and pelvic obliquity.
It can guide intraoperative traction and instrumentation strategy by identifying curves requiring greater distraction.
On the convex side, the distance is typically larger; measurement should be taken on the concave (compressed) side for consistency.
In severe neuromuscular or degenerative scoliosis, restoration of ≥ 2–3 cm of rib–pelvis space intraoperatively often corresponds to improved sitting balance and pain reduction.
When using EOS or stitched long-cassette radiographs, ensure true coronal alignment (no rotation) for reproducibility.
MRI or CT may further delineate rib impingement or costovertebral deformity in preoperative planning.