Image Type
Apical Vertebral Translation (AVT)
1) Description of Measurement
The Apical Vertebral Translation (AVT) quantifies the lateral displacement of the apical vertebra from the central vertical axis of the body in the coronal plane.
It provides an objective measure of the severity of scoliotic curvature and the degree of spinal asymmetry.
The apical vertebra is defined as the most laterally deviated and rotated vertebra at the midpoint of a spinal curve.
AVT helps assess curve flexibility, progression, and surgical correction and is routinely reported alongside the Cobb angle and coronal balance in scoliosis evaluation.
2) Instructions to Measure
Obtain a standing full-length PA or AP spine X-ray, ensuring the patient’s head and pelvis are level and centered.
Identify the apical vertebra of the curve — the vertebra most laterally displaced from the midline.
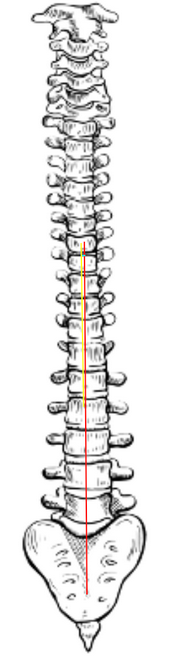
Draw the Central Sacral Vertical Line (CSVL):
Identify the center of the sacrum (S1 endplate midpoint).
Draw a vertical plumb line extending upward through this point to the top of the image.
Mark the center of the apical vertebral body (midpoint between the lateral borders of its endplates).
Measure the horizontal distance (in millimeters) between the center of the apical vertebra and the CSVL.
This distance is the Apical Vertebral Translation (AVT).
If multiple curves are present, measure AVT for each curve (thoracic, thoracolumbar, lumbar).
The direction of translation should be noted — right (positive) or left (negative) relative to the CSVL.
3) Normal vs. Pathologic Ranges
Normal/balanced alignment: ≤ 10 mm; no significant coronal deviation
Mild translation: > 10-20 mm; may indicate early or compensatory curvature
Moderate translation: > 20-40 mm; correlates with progressive or structural scoliosis
Severe translation: > 40 mm; significant deformity, often a surgical indication
Key Points:
AVT is frequently correlated with Cobb angle magnitude — larger Cobb angles generally yield higher AVT values.
Improvement in AVT postoperatively reflects successful correction of coronal deformity and re-centering of the trunk over the pelvis.
4) Important References
Cobb JR. Outline for the study of scoliosis. In: Instructional Course Lectures. Vol 5. American Academy of Orthopaedic Surgeons; 1948:261–275.
Lenke LG, Betz RR, Harms J, et al. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am. 2001;83(8):1169–1181.
Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR. Coronal and sagittal balance in idiopathic scoliosis: does correction correlate with improvement in pain and function? Spine. 2005;30(7):682–688.
Hwang SW, Samdani AF, Cahill PJ, et al. Apical vertebral translation and coronal balance after selective thoracic fusion in adolescent idiopathic scoliosis. Spine. 2011;36(24):E1619–E1625.
Newton PO, Faro FD, Gollogly S, et al. Results of preoperative flexibility assessment in adolescent idiopathic scoliosis: are we doing enough? Spine. 2007;32(25):2658–2664.
5) Other info....
AVT provides a linear measure of coronal deformity, complementing angular measurements such as the Cobb angle.
It is especially useful in evaluating curve flexibility during bending radiographs and postoperative correction following instrumentation.
Positive AVT values indicate rightward translation; negative AVT indicates leftward deviation.
Multiple curve patterns (double major or triple curve scoliosis) may have distinct AVTs for each segment.
EOS imaging or stitched long-cassette digital radiographs are preferred for accurate measurement and reduced distortion.
AVT should always be interpreted in conjunction with coronal balance, pelvic tilt, and shoulder alignment to assess global posture.
In surgical planning, AVT helps guide fusion level selection and implant placement strategy to restore symmetry and balance.