Image Type
T1 Pelvic Angle (T1PA)
1) Description of Measurement
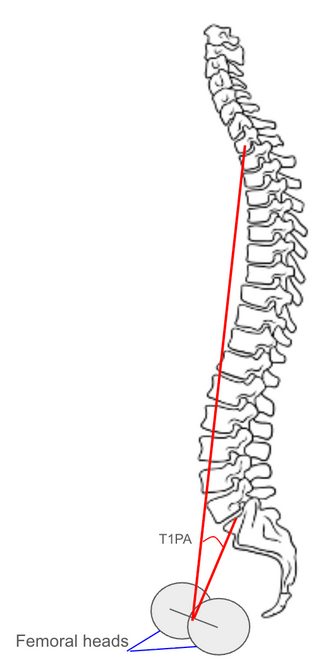
The T1 Pelvic Angle (T1PA) is a composite radiographic parameter that evaluates global sagittal alignment by incorporating both spinal inclination and pelvic retroversion into a single angular measure.
It is defined as the angle between two lines: one drawn from the center of the T1 vertebral body to the center of the femoral heads, and the other from the center of the S1 endplate to the center of the femoral heads.
Unlike the Sagittal Vertical Axis (SVA), which is highly dependent on patient positioning, the T1PA provides a posture-independent assessment of sagittal alignment and is thus a more reliable marker for overall spinal balance.
An increased T1PA corresponds to greater anterior spinal inclination and compensatory pelvic retroversion — key indicators of positive sagittal imbalance.
2) Instructions to Measure
Obtain a standing lateral full-length spine X-ray with the patient standing upright, knees fully extended, and arms supported forward at shoulder height.
Identify the following anatomical landmarks:
Center of the T1 vertebral body (midpoint between the anterior and posterior cortices of T1).
Center of the femoral heads (use the midpoint if they are superimposed; if not, use the midpoint of the line joining both centers).
Center of the S1 endplate (midpoint of the superior sacral endplate).
Draw:
Line 1: from the center of T1 to the center of the femoral heads.
Line 2: from the center of S1 endplate to the center of the femoral heads.
Measure the angle formed between these two lines — this is the T1 Pelvic Angle (T1PA).
A larger angle indicates greater sagittal malalignment due to combined forward trunk lean and pelvic retroversion.
Record the T1PA in degrees (°).
3) Normal vs. Pathologic Ranges
Normal T1PA: < 10°; balanced sagittal alignment; minimal compensatory pelvic retroversion
Mild sagittal imbalance: 10-20°; early compensation by pelvis and thoracic curvature
Moderate sagittal imbalance: 20-30°; associated with increased energy expenditure and postural strain
Severe sagittal imbalance: > 30°; marked anterior translation of the trunk; commonly associated with spinal deformity or flat-back syndrome
Key Point:
T1PA > 20° is generally considered a clinically significant threshold for sagittal malalignment and correlates strongly with patient-reported disability (ODI > 40%).
4) Important References
Protopsaltis TS, Lafage V, Vira S, et al. T1 pelvic angle (TPA): a novel radiographic measure of global sagittal deformity accounts for both spinal inclination and pelvic retroversion. Spine. 2014;39(9):782–788.
Lafage R, Schwab F, Challier V, et al. Defining spino-pelvic alignment thresholds correlated with quality of life in adult spinal deformity: standing alignment. Spine. 2016;41(1):62–69.
Schwab FJ, Lafage V, Boyce R, Skalli W, Farcy JP. Gravity line analysis in adult volunteers: age-related correlation with spinal and pelvic parameters. Spine. 2006;31(25):E959–E967.
Le Huec JC, Thompson W, Mohsinaly Y, Barrey C, Faundez A. Sagittal balance of the spine. Eur Spine J. 2019;28(9):1889–1905.
Diebo BG, Oren JH, Lafage V, et al. Global spinal alignment in the setting of cervical deformity: importance of head position and pelvic compensation. Spine. 2016;41(19):1591–1598.
5) Other info....
The T1 Pelvic Angle (T1PA) integrates both SVA (spinal inclination) and pelvic tilt (pelvic compensation), providing a more comprehensive and stable representation of sagittal balance.
It is less affected by patient posture or knee flexion, making it highly reliable for comparing pre- and postoperative images.
T1PA is particularly useful in adult spinal deformity surgery planning, as it correlates with functional outcomes and energy-efficient posture restoration.
It should be analyzed in conjunction with pelvic incidence (PI), lumbar lordosis (LL), and PI–LL mismatch to assess spinopelvic harmony.
In general, T1PA ≤ PI + 10° is considered an optimal surgical alignment target to maintain physiologic posture and improve quality of life.
Large T1PA values (>30°) indicate decompensation, often associated with fatigue, pain, and decreased quality of life.
EOS imaging or stitched low-dose long-cassette radiographs provide superior accuracy for T1PA measurement by minimizing projection error.