Image Type
Sacral Morphometry
1) Description of Measurement
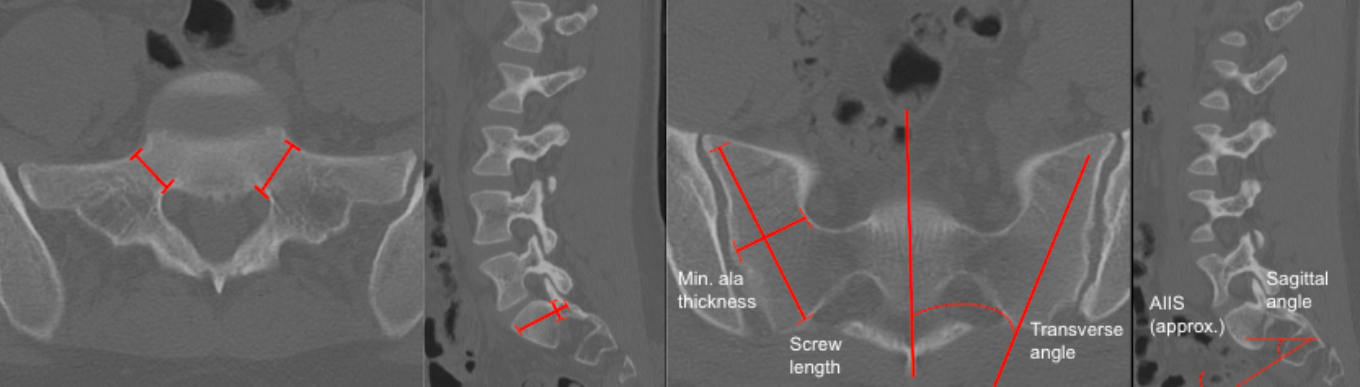
Sacral morphometry defines the osseous corridors available for S1 pedicle screws and S1/S2 alar-iliac (SAI) screws, ensuring safe trajectories that avoid neural foramina, sacral canal, and pelvic viscera while maximizing fixation strength. Measurements include:
S1 pedicle width & height
Sacral ala thickness
Alar-iliac corridor length
Transverse (medial-lateral) and sagittal (cephalocaudal) trajectory angles
These measurements are critical for preoperative planning of pelvic fixation in deformity, trauma, and revision surgery.
2) Instructions to Measure
A. S1 Pedicle Morphometry
Axial CT (through S1 pedicles):
Identify the narrowest portion of the S1 pedicle.
Measure:
Pedicle Width (mm): Medial–lateral cortical distance.
Sagittal CT:
Measure pedicle length from posterior cortex of sacrum to anterior vertebral body cortex along the pedicle axis.
Pedicle Height (mm): Superior–inferior diameter.
B. Sacral Ala / SAI Corridor
Axial CT (through S1 or S2 ala):
Identify the starting point:
S1AI: 1–2 mm inferior and lateral to S1 dorsal foramen.
S2AI: Midpoint between S1 and S2 dorsal foramina.
Draw trajectory toward the AIIS (anterior inferior iliac spine).
Measure:
Minimum ala thickness (narrowest corridor).
Transverse angle (medial to lateral angulation).
Sagittal CT:
Measure:
Sagittal angle (caudal inclination toward AIIS).
Maximum screw length from sacral entry to anterior iliac cortex.
3) Normal vs. Pathologic Ranges
S1 Pedicle Width
Typical Adult Range: 10 - 15 mm
Pathologic/High-Risk: < 8 mm = unsafe for standard 7 - 7.5 mm screw
S1 Pedicle Height
Typical Adult Range: 12 - 18 mm
Pathologic/High-Risk: < 10 mm = risk of breach
Sacral Ala Thickness
Typical Adult Range: 12 - 20 mm
Pathologic/High Risk: < 10 mm = high breach risk
S2AI Screw Length
Typical Adult Range: 70 - 90 mm
Pathologic/High Risk: < 60 mm = limited pelvic fixation
Transverse Angle
Typical Adult Range: 30-40° lateral
Pathologic/High Risk: < 20° or > 50° = breach risk
Sagittal Angle
Typical Adult Range: 20-40° caudal
Pathologic/High Risk: Excessive caudal -> sciatic notch risk
4) Important References
Yilmaz E, Abdul-Jabbar A, Tawfik T, et al. S2 Alar-Iliac Screw Insertion: Technical Note with Pictorial Guide. World Neurosurg. 2018 May;113:e296-e301. doi: 10.1016/j.wneu.2018.02.009. Epub 2018 Feb 10.
O'Brien JR, Yu WD, Bhatnagar R, et al. An anatomic study of the S2 iliac technique for lumbopelvic screw placement. Spine (Phila Pa 1976). 2009 May 20;34(12):E439-42. doi: 10.1097/BRS.0b013e3181a4e3e4.
Kebaish KM. Sacropelvic fixation: techniques and complications. Spine (Phila Pa 1976). 2010 Dec 1;35(25):2245-51. doi: 10.1097/BRS.0b013e3181f5cfae.
Jain A, Brooks JT, Kebaish KM, Sponseller PD. Sacral Alar Iliac Fixation for Spine Deformity. JBJS Essent Surg Tech. 2016 Mar 9;6(1):e10. doi: 10.2106/JBJS.ST.15.00074.
5) Other info....
S2AI screws provide lower profile fixation and reduce wound complications compared with traditional iliac bolts.
Always assess neural foramina, sacral canal, and sciatic notch proximity before finalizing trajectory.
In dysplastic sacra or severe deformity, 3-D navigation is strongly recommended.
Adapted from: Feger J, Campos A, Murphy A, et al. CT lumbar spine (protocol). Reference article, Radiopaedia.org (Accessed on 03 Jan 2026) https://doi.org/10.53347/rID-90041